A Leading Cause of Death Worldwide, Scarce Treatment Options
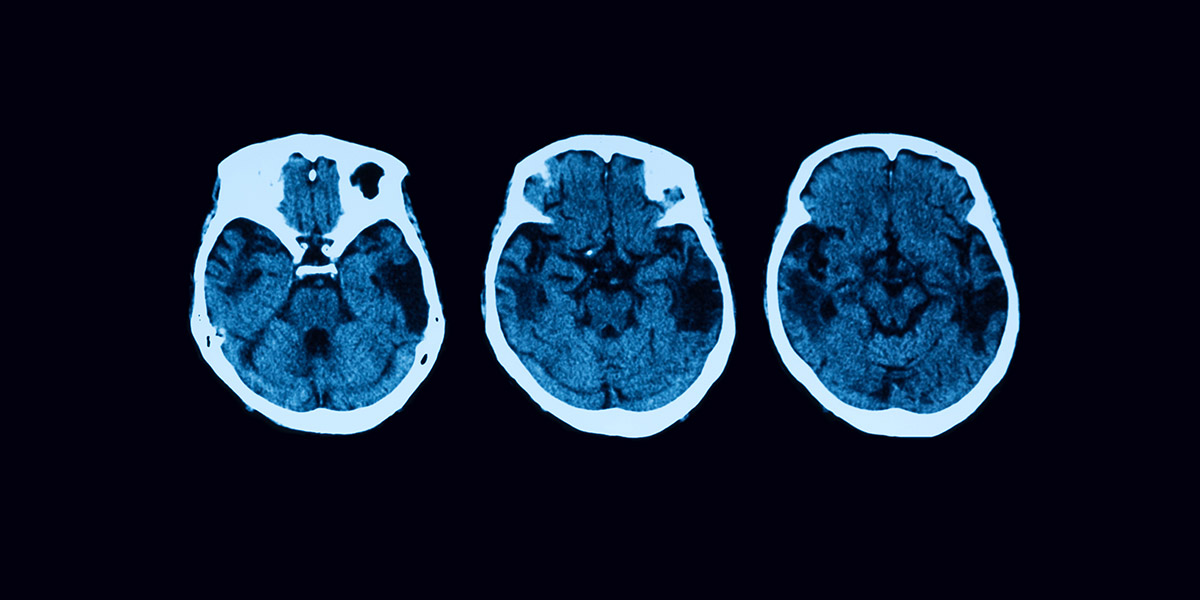
Patients that suffer a stroke can have a range of impairments, including paralysis, vision and speech loss, and even death.1 Several factors contribute to the risk of stroke, including tobacco use, a sedentary lifestyle, diabetes, high blood pressure, and elevated levels of cholesterol and triglycerides in the blood. Worldwide, stroke is the second most common cause of death and the third most common cause of morbidity. 2 One stroke occurs every 40 seconds in the United States, resulting in a death rate of approximately 20%.1 Ischemic stroke accounts for approximately 87% of all strokes and occurs when a vessel supplying blood to the brain is blocked, primarily by fatty plaque deposits that can line the vessel wall.3
Despite its severity and widespread impact, there are currently only two FDA approved treatments for treating ischemic stroke. Unfortunately, these treatments are time sensitive and can only be used during the first 24 hours after the patient has shown symptoms of a stroke, limiting their application to less than 20% of all stroke patients.4,5 Furthermore, these are acute treatments that only aid in restoring the flow of blocked blood vessels and do not repair the tissue that was damaged by the stroke. Several studies have evaluated therapies promoting endogenous tissue repair using pharmacological approaches or trophic factors, but they were largely ineffective.6
Limitations of Current Cell Therapies
Cell-based therapies are a promising option for resolving stroke-induced cellular deficits when implemented within days after a stroke. Progenitor-based vascular cell therapies have been demonstrated to improve neurological recovery by exploiting neurogenic and vasculogenic processes that occur during nerve tissue repair and development. Unfortunately, current approaches face significant obstacles due to reliance on scarce or impaired progenitor cell populations, especially in patients with multiple diseases. These therapies also carry additional risks such as uncontrolled differentiation, tumorigenesis, genetic abnormalities, and immunogenicity.
New breakthroughs in direct cell reprogramming have unlocked the possibility of developing patient-specific cell therapies that overcome the obstacles mentioned above by using abundant and readily available cell sources, such as skin fibroblasts. However, current gene delivery methods used to directly reprogram cells are far from ideal. Viral transduction has biosafety concerns and capsid size constraints on gene payload. Physical delivery methods, such as biolistic transfection, can cause extensive cell damage and negatively affect cell function. Chemical transfection methods, such as lipo/polyplex-based nanocarriers, rely significantly on endocytosis to deliver genetic information, making them less effective if endosomal escape of the cargo is not efficient. Bulk electroporation (BEP) is a quick and easy method for gene delivery, but the technique also relies on endocytosis and requires a high-magnitude, non-uniform voltage that often results in poor cell health.
A Novel Solution: Nanotransfection-Based Cell Reprogramming
A study published in Science Advances in 2021 set out to resolve the major challenges associated with current gene delivery technologies and direct cell reprogramming by utilizing a novel and simple nano-transfection based method for non-viral cell reprogramming.7 The study by Lemmerman et al. used the ZymoPURE II Plasmid Midiprep Kit to purify endotoxin-free plasmids containing the developmental transcription factor genes Etv2, Foxc2, and Fli1. Mouse fibroblasts were then transfected with the plasmid cocktail using a nanochannel-driven delivery system, a delivery technique that applies an electric field through arrayed microchannels to directly deliver plasmids to cells. 8 Nano-transfection enables the direct cytosolic delivery of reprogramming-factors, without the adverse side effects associated with BEP and viral transfections described above. Transfected fibroblasts were injected intracranially to investigate the effect on cerebral vasculature and functional recovery after stroke.
It was found that delivery of the reprogrammed fibroblasts into a mouse model of ischemic stroke resulted in dose-dependent increases in perfusion, reduced stroke volume, and significant improvement of locomotive skills in stroke-affected mice. Further analysis also confirmed that the treatment increased vascularity and neuronal cellularity and reduced glial scar formation. The promising results of this study suggest that vasculogenic cell reprogramming using a nonviral nano-transfection gene delivery system is a feasible approach for treating ischemic stroke.
Citations
- Virani, S. S., Alonso, A., Benjamin, E. J., Bittencourt, M. S., Callaway, C. W., Carson, A. P., Chamberlain, A. M., Chang, A. R., Cheng, S., Delling, F. N., Djousse, L., Elkind, M. S. V., Ferguson, J. F., Fornage, M., Khan, S. S., Kissela, B. M., Knutson, K. L., Kwan, T. W., Lackland, D. T., Lewis, T. T., Lichtman, J. H., Longenecker, C. T., Loop, M. S., Lutsey, P. L., Martin S. S., Matsushita, K., Moran, A. E., Mussolino, M. E., Perak, A. M., Rosamond, W. D., Roth, G. A., Sampson, U. K. A., Satou G. M., Schroeder, E. B., Shah, S. H., Shay, C. M., Spartano, N. L., Stokes, A., Tirschwell, D. L., VanWagner, L. B., Tsao, C. W. (2020) American Heart Association Council on Epidemiology and Prevention Statistics Committee and Stroke Statistics Subcommittee, Heart disease and stroke statistics—2020 update: A report from the american heart association. Circulation 141(9), e139 – e596.
- Johnson, W., Onuma, O., Owolabi, M., Sachdev, S. (2016) Stroke: A global response is needed. Bull. World Health Organ. 94(9), 634 – 634A.
- American Stroke Association. Ischemic Stroke (Clots). Retrieved June 10th, 2024, from https://www.stroke.org/en/about-stroke/types-of-stroke/ischemic-stroke-clots
- National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group, Tissue plasminogen activator for acute ischemic stroke. (1995) N. Eng. J. Med. 333(24), 1581 – 1588.
- Hacke, W., Kaste, M., Bluhmki, E., Brozman, M., Dávalos, A., Guidetti, D., Larrue, V., Lees, K. R, Medeghri, Z., Machnig, T., Schneider, D., von Kummer, R., Wahlgren, N., Toni, D., ECASS Investigators. (2008) Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N. Engl. J. Med. 359(13), 1317 – 1329.
- Zhao, L.R., Willing, A. (2018) Enhancing endogenous capacity to repair a stroke-damaged brain: An evolving field for stroke research. Prog. Neurobiol. 163 - 164, 5 – 26.
- Lemmerman, L. R., Balch, M. H. H., Moore, J. T., Alzate-Correa, D., Rincon-Benavides, M. A., Salazar-Peurta, A., Gynawali, S., Harris, H. N., Lawrence, W., Ortega-Pineda, L., Wilch, L. Risser, I. B., Maxwell, A. J., Duarte-Sanmiguel, S., Dodd, D., Guio-Vega, G. P., McTigue, D. M., Arnold, W. D., Nimjee, S. M., Sen, C. K., Khanna, S., Rink, C., Higuita-Castro, N., Gallego-Perez, D. (2021) Nanotransfection-based vasculogenic cell reprogramming drives functional recovery in a mouse model of ischemic stroke. Science Advances 7(12), eabd4735.
- Gallego-Perez, D., Pal, D., Ghatak, S., Malkoc, V., Higuita-Castro, N., Gnyawali, S., Chang, L., Liao, W. C., Shi, J., Sinha, M., Singh, K., Steen, E., Sunyecz, A., Stewart, R., Moore, J., Ziebro, T., Northcutt, R. G., Homsy, M., Bertani, P., Lu, W., Roy, S., Khanna, S., Rink, C., Sundaresan, V. B., Otero, J. J., Lee, L. J., Sen, C. K. (2017) Topical tissue nano-transfection mediates non-viral stroma reprogramming and rescue. Nature Nanotechnology 12(10), 974 – 979.